Subscribe to the newsletter
Get emailed whenever a new video, article, or course is released. This gives you instant access to all of our fresh content.
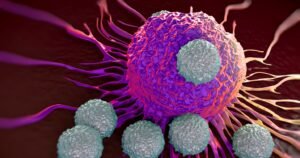
Last week, the field of cancer immunotherapy reached a pretty exciting milestone with Allogene Therapeutics’ publication of Phase 1 results from their ALPHA/ALPHA2 trials, which evaluated cema-cel, their allogeneic CD19-targeting CAR T-cell therapy, in patients with relapsed/refractory large B cell lymphoma (r/r LBCL).
Here’s what you need to know.
What is cema-cel?
Unlike autologous CAR T-cell therapies, which require the harvesting and genetic engineering of a patient’s own T cells, cema-cel is an “off-the-shelf” product that is derived from healthy donors.
Allogene then takes these donor-derived T cells and does three things:
i) they inhibit the proper expression of the T cell receptor (by disrupting the TRAC locus) to prevent graft-versus-host disease (GvHD),
ii) they express a CD19-targeting CAR to enable B cell targeting (stock standard for a CAR-T platform), and
iii) they delete CD52 – now, this is interesting. Allogene is pursuing a unique lymphodepletion regimen that includes a CD52-targeting antibody (ALLO-647)that will target and aid in the elimination of potential alloreactive host T cells (T cells express high levels of CD52 on their surface). To make cema-cel resistant to this, they delete CD52 – pretty cool.
Due to their donor-derived nature, cema-cel is able to be manufactured in advance, cryopreserved, and made immediately available for infusion. In the ALPHA/ALPHA2 trials, the median time from patient enrollment to CAR-T infusion was just 5 days, a stark contrast to the lengthy wait times (usually 4-6 weeks, minimum) associated with autologous therapies.
Key Findings from the Phase 1 Trials
Okay, here’s what they found – I’ll make it short and sweet.
As for safety, no cases of GvHD, high-grade cytokine release syndrome (CRS), or immune effector cell-associated neurotoxicity syndrome (ICANS) were reported. Adverse events were primarily hematologic and (likely) associated with lymphodepletion, which is expected for adoptive cell therapies.
Accessibility? Well, the rapid turnaround time (median of 5 days from enrollment to cell infusion) eliminates the need for bridging therapy, which is a huge advantage for patients with aggressive disease who cannot afford delays.
And finally, efficacy. The selected Phase 2 dosing regimen (flu/cyclo + 90 mg ALLO-647 for 3 days –> cema-cel infusion) achieved a 67% overall response rate (ORR) and a 58% complete response (CR) rate. Importantly, responses were durable, with a median duration of response (DOR) of 23.1 months in the patients that achieved CRs.
Importantly, cema-cel achieved a CR rate of 100% in patients with low tumor burden (<1000 mm² SPD) or normal lactate dehydrogenase levels, suggesting that it may perform particularly well in minimal residual disease (MRD) settings.
How Does It Compare to Autologous CAR T-Cell Therapies?
Cema-cel’s efficacy numbers (OR/CR of 67%/58% in phase 2 dosing cohort) are comparable to those of approved autologous CAR T-cell products like axi-cel and tisa-cel, which report ORRs of 66–80% and CR rates of 42–60% (reference). However, being an “off-the-shelf” option, cema-cel offers significant logistical advantages including i) faster treatment initiation, ii) less intense lymphodepletion (due to the inclusion of ALLO-647), and iii) no reliance on patient-specific manufacturing, reducing variability and failure risks.
These benefits make allogeneic CAR T-cell therapy particularly appealing for patients who are ineligible for or unable to wait for autologous options.
What's Next?
The promising results from the ALPHA/ALPHA2 trials pave the way for pivotal studies like the ongoing ALPHA3 Phase 2 trial, which is exploring cema-cel as a consolidation therapy in patients with MRD after first-line chemoimmunotherapy.
If successful, this could redefine treatment for LBCL by enabling quick infusion of an immediately available CAR-T therapy to go in as a “clean-up crew” to prevent recurrence due to MRD.
Important Links
Allogene’s Press Release: https://ir.allogene.com/news-releases/news-release-details/allogene-therapeutics-announces-publication-durable-response
Published results: https://ascopubs.org/doi/pdf/10.1200/JCO-24-01933
Recent Videos
Recent Articles
LATEST IN ONCOLOGY BIOTECH
PD-1 Biosimilar Races Towards Approval: What This Means For Oncology
AbbVie and Xilio Partner Up to Advance Tumor-Activated T Cell Engagers
NKGen’s FDA Fast Track & Positive Alzheimer’s Results: A Win For NK Cells